Background:
Patients with essential thrombocythemia (ET) are burdened with an increased risk of thrombosis and disease transformation, both significant contributors to morbidity and mortality. However, based on the available literature, there are limited tools available to predict the development of these complications. Particularly, the association between hematologic parameters and thrombosis is unclear, making risk stratification and disease management challenging. Utilizing a large retrospective database, we assessed the impact of hematocrit (Hct), red blood cell count (RBC), white blood cell count (WBC), and platelet count (Plt) on the subsequent development of thrombosis and disease transformation to myelofibrosis (MF), polycythemia vera (PV), and acute leukemia.
Methods:
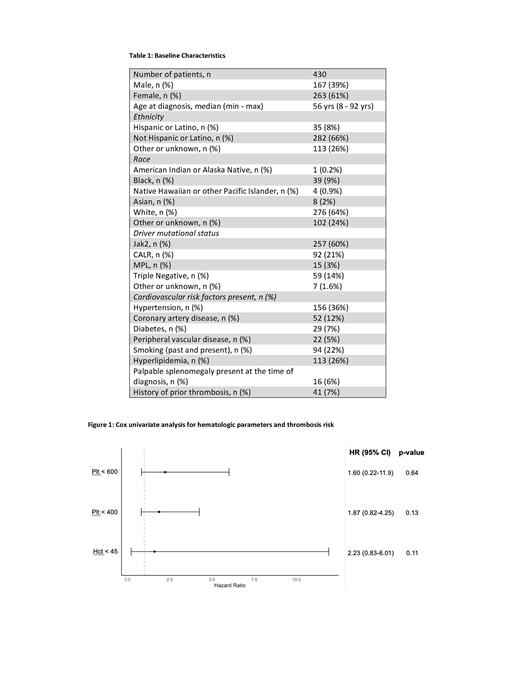
We included ET patients treated at our institution between 2007 and 2021. The index time was date of diagnosis or date of first contact at Mount Sinai Hospital for patients with a prior history of ET. Hematologic parameters (Hct, RBC, WBC, Plt) were documented at three-month intervals after the index time. Patients were included in the study if they had at least three sets of laboratory values prior to the outcome of interest.
For each hematologic parameter, we performed univariate cox analysis of time to thrombosis or progression to either MF, PV, or acute leukemia. Each lab parameter was analyzed as a time dependent covariate, taking into account the length of time the patient was above or below the threshold of interest. Hct and plt were specifically evaluated as dichotomous variables, with a cut off of less than or greater than 45% for Hct based on CYTO-PV results. For plt, two cut-off values were used: less than or greater than 400 (based on ELN response criteria) and less than or greater than 600 (based on Cortelazzo et al HU treatment goal) in plt/microliter.
Results:
We identified 430 patients who met criteria and were included in the analysis. Our cohort of patients was mostly female (61%), non-Hispanic (66%), white (64%), JAK2 mutated (60%), with an average age at diagnosis of 56 years and a median follow-up time of 33 months. 41 (7%) patients had a history of prior thrombosis. There was a total of 23 major thromboses that occurred after the index time with 12 venous and 11 arterial thrombotic events. 38 patients progressed to post ET-MF, 20 patients developed post ET-PV, and 10 patients transformed to acute leukemia.
For the assessment of thrombotic risk, there were no significant associations between any of the hematologic parameters and this outcome. We also evaluated the risk of thrombosis in the JAK2 positive subset of patients (n of 15), and did not find any significant association with any of the lab parameters (in particular, for hct < 45%, p > 0.99). For transformation to MF, plt < 400 x10 9/L was associated with an increased risk of the development of post-ET MF (HR 2.2, p 0.016), and the same was seen with plt < 600 x10 9/L (HR 2.2, p 0.044). The development of PV was less likely with a hct lower than 45% (HR 0.03, p < 0.001), with similar results seen for plt < 400 x10 9/L (HR 0.2, p 0.03) and plt < 600 x10 9/L (HR 0.2, p 0.002). For transformation to acute leukemia, plt < 400 x10 9/L (HR 8.3, p 0.008) was associated with an increased risk of this complication.
Conclusions:
In this retrospective cohort of 430 patients with ET, we found no associations between four different hematologic parameters over time with thromboses. In particular, this data once again argues against aiming to achieve a particular platelet goal to minimize thrombosis in ET patients. The lack of association between hematologic parameters and thrombotic risk was similarly exemplified in our subset of JAK2 mutated ET patients. Pertaining to disease transformation, plt count appeared to be the most predictive out of all of the parameters, with lower plt values corresponding to increased risk of both post-ET MF and acute leukemia, which both warrant further exploration. A hct level of less than 45% appeared to be protective against the development of post-ET PV. Significant limitations of our study include the retrospective nature as well as the small number of events of interest that our patients experienced. Future studies must continue to focus on surrogate endpoint validation in order to more reliably predict thrombotic events as well as disease progression in patients with ET given the significant morbidity and mortality that such events incur.
Disclosures
Kremyanskaya:Protagonist Therapeutics, Inc.: Consultancy, Research Funding. Hoffman:Dompe: Patents & Royalties; Summitomo: Research Funding; Kartos Abbvie: Research Funding; Curis: Research Funding; TD2: Research Funding; Karyopharm: Research Funding; Dexcel Pharma: Research Funding; Silence Therapeutics: Consultancy; Cellinkos: Consultancy; Protagonist Therapeutics: Consultancy. Mascarenhas:Incyte, Novartis, Roche, Geron, GSK, Celgene/BMS, Kartos, AbbVie, Karyopharm, PharmaEssentia, Galecto, Imago, Sierra Oncology, Pfizer, MorphoSys, CTI Bio: Consultancy; Bristol Myers Squibb, Celgene, Constellation Pharmaceuticals/MorphoSys, CTI BioPharma, Galecto, Geron, GSK, Incyte Corporation, Karyopharm Therapeutics, Novartis, PharmaEssentia, Prelude Therapeutics, Pfizer, Merck, Roche, AbbVie, Kartos: Consultancy, Membership on an entity's Board of Directors or advisory committees; AbbVie, Bristol Myers Squibb, Celgene, CTI BioPharma, Geron, Incyte Corporation, Novartis, Janssen, Kartos Therapeutics, Merck, PharmaEssentia, Roche: Research Funding; Bristol Myers Squibb, Celgene, CTI BioPharma, Geron, Incyte Corporation, Janssen, Kartos Therapeutics, Merck, Novartis, PharmaEssentia, Roche; Participated in consulting or advisory committees - AbbVie, Bristol Myers Squibb, Celgene, Constellation Pharmac: Research Funding; GSK: Honoraria; AbbVie, CTI BioPharma Corp, a Sobi company, Geron, GlaxoSmithKline, Imago, Incyte, Kartos, Kayropharm, MorphoSys, Novartis, Pfizer, PharmaEssentia, Sierra: Consultancy. Tremblay:GSK: Consultancy; Sierra Oncology: Consultancy; Astellas Pharma: Research Funding; Gilead: Research Funding; Cogent Biosciences: Consultancy; AbbVie: Consultancy; Novartis: Consultancy; CTI Biopharma: Consultancy, Research Funding.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal